HHV6, a human herpes virus discovered in the mid-eighties, is active in nearly all Lyme disease patients along with borrelias Burgdorferi, the infamous bacteria known to cause Lyme. Though often referred to as a co-infection, HHV6 is not transmitted with the Lyme infection. The human herpes virus (HHV6) is opportunistic, and lays inactive in hosts waiting for the moment of least environmental resistance to strike. A Lyme infection is one such opportunity HHV6 commonly takes to present itself.
There are two variations of the human herpes virus known as HHV-6A and HHV-6B. Nearly identical, the two virus strains differ only in their activation cycles within the host.
HHV-6A
This particular strain of HHV-6 is commonly found in patients with Lyme disease, Chronic Fatigue Syndrome (CFS), Multiple Sclerosis (MS), AIDS, and Cancer. Most often it strikes within an adult host and is associated with neurological symptoms and fatigue.
HHV6B
Affecting nearly 100% of children by the age of two, it commonly presents with fever and encephalitis in infants. Reactivation of HHV-6B can also occur in patients of all ages who have received a transplant. The B strain of HHV6 is characterized by mild flu-like symptoms and rash in some cases. Progression of this strain is accompanied by high fever, encephalitis and even seizures. In most cases, and after the initial activation, the virus lies dormant or latent. Reactivation of HHV6B occurs in 4% of transplant patients causing complications such as encephalitis, pneumonitis and liver failure.
Differences In The HHV6A and HHV6B Virus Strains
Though nearly identical, there are differences in epidemiology and pathogenicity of the two strains. HHV-6B is acquired in early childhood (often in daycare centers), infecting up to 90% of most populations during infancy, while HHV-6A, is generally not seen until adulthood. Both versions of the virus can be found in saliva and are assumed to be spread this way as well.
Dangers Associated With HHV6
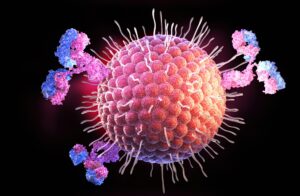
HHV-6 is of greatest concern to immunocompromised patients with a high HHV6 viral load, especially those who have had organ or bone marrow transplants, those who are HIV positive, and those with chronic Lyme disease complex. By attacking a number of cells in the body which aid its ability to fight off disease and infection, HHV6 is immune suppressive and can activate other viruses in the process.
HHV6 Attacks the Following Healthy Cells in the Human Body
-
- CD 4 lymphocytes
-
- NKTs
-
- Oligodedrocytes
-
- CD8 cells
-
- Microglial cells
Pink areas indicate HHV6 infection thru a staining process
Though HHV-6 lies dormant for long periods of time, once reactivated, infection can occur quickly. During its dormancy the virus waits in salivary glands, kidneys or the brain until it is reactivated.
Connection to Cancer
Since more and more research continues to uncover a link between viruses and chronic illness including many cancers, HHV6 is at the forefront of continued study. Its link to cancer comes via a protein called P53 which regulates the cell cycle and acts as a tumor suppressor. HHV6 is known to attack this particular protein and is often found active in cancer patients.
The Herpes-Cancer Connection: What the Research Says
- Herpes and Cervical Cancer
One of the most well-established links between herpes and cancer relates to cervical cancer. However, it’s crucial to note that this connection is specific to the human papillomavirus (HPV), a sexually transmitted infection distinct from HSV. While both viruses can cause genital sores, HPV is the primary cause of cervical cancer.
- Herpes and Kaposi’s Sarcoma
Kaposi’s sarcoma, a rare form of cancer that develops in the lining of blood and lymph vessels, has been linked to herpes simplex virus type 8 (HSV-8), also known as Kaposi’s sarcoma-associated herpesvirus (KSHV). This virus is different from the HSV-1 and HSV-2 strains commonly associated with oral and genital herpes. While HSV-8 is a contributing factor to Kaposi’s sarcoma, it typically affects individuals with compromised immune systems or autoimmune disorders.
- Herpes and Other Cancers
Studies have suggested potential associations between herpes and other types of cancer, such as oral and prostate cancer. Many factors, including lifestyle choices, genetic predisposition, and other health conditions, can influence an individual’s cancer risk.





